Organizing your kitchen for a low FODMAP diet can significantly improve your quality of life if you suffer from irritable bowel syndrome (IBS) or other gastrointestinal issues. A well-structured kitchen stocked with appropriate foods and ingredients is essential for successfully following this dietary approach and managing symptoms. By creating an environment that supports your nutritional needs, you can more easily adhere to the diet and potentially experience relief from digestive discomfort.
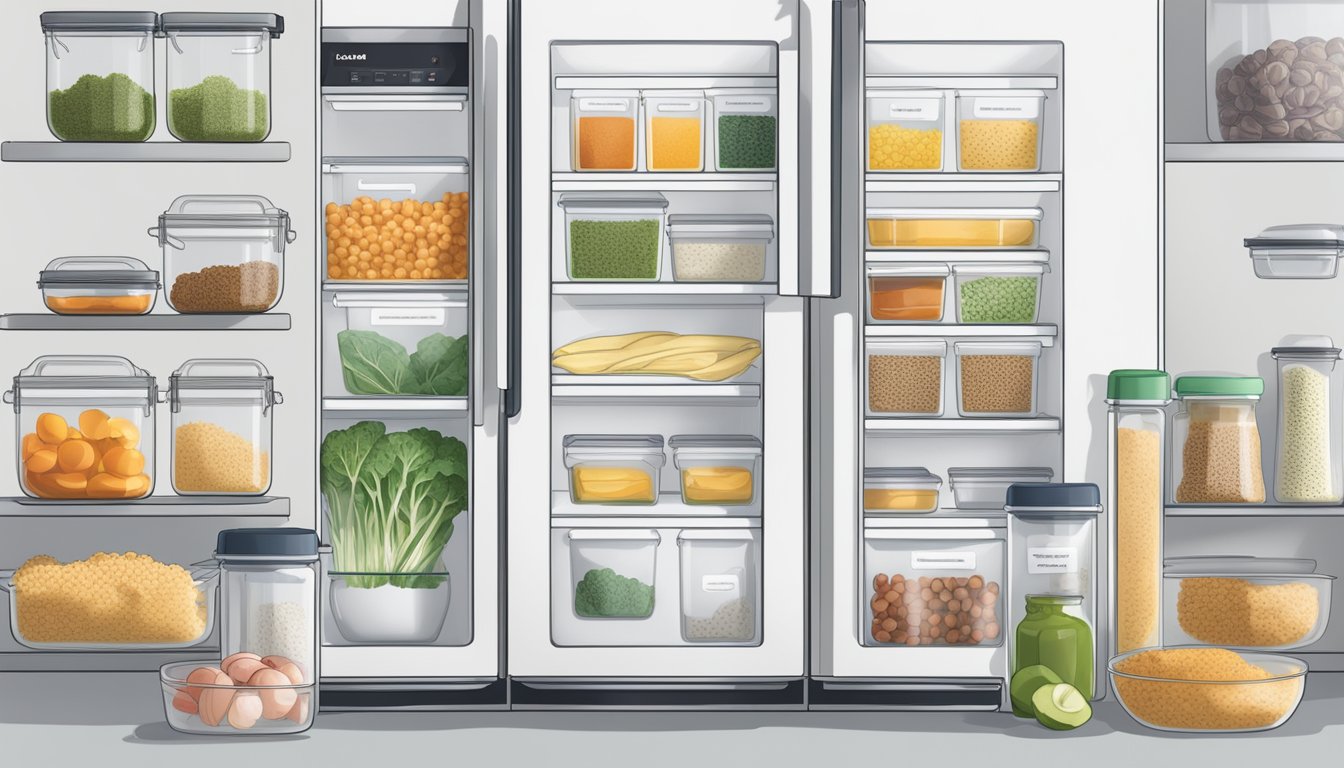
The low FODMAP diet involves eliminating certain fermentable carbohydrates that can trigger IBS symptoms. This process requires careful planning and organization to ensure you have access to suitable alternatives. Stocking your pantry with low FODMAP staples such as rice, quinoa, and gluten-free oats, as well as organizing your refrigerator with lactose-free dairy products and low FODMAP fruits and vegetables, can streamline meal preparation and reduce the temptation to consume problematic foods.
Implementing an effective organization system in your kitchen can make following the low FODMAP diet more manageable and less overwhelming. By clearly labeling foods, designating specific areas for low FODMAP items, and keeping trigger foods separate or out of sight, you can create a supportive environment that promotes dietary adherence and potentially leads to improved gastrointestinal health.
Understanding Low FODMAP Diet and IBS
The Low FODMAP diet is a specialized eating plan designed to manage symptoms of Irritable Bowel Syndrome (IBS). It involves carefully selecting foods to reduce digestive distress and improve gut health.
What is a Low FODMAP Diet?
A Low FODMAP diet restricts certain carbohydrates that can trigger digestive issues. FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are types of carbohydrates that some people have difficulty digesting.
The diet aims to reduce intake of high FODMAP foods like certain fruits, vegetables, dairy products, and grains. Low FODMAP alternatives are emphasized instead.
Following this diet requires careful food selection and label reading. A comprehensive FODMAP food list is an essential tool for those embarking on this dietary plan.
Basics of Digestive Disorders and IBS
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder affecting the large intestine. It causes symptoms such as abdominal pain, bloating, gas, and changes in bowel habits.
IBS is classified as a functional disorder, meaning there’s no visible damage to the digestive tract. However, its symptoms can significantly impact quality of life.
Other digestive disorders include:
- Inflammatory Bowel Disease (IBD)
- Celiac Disease
- Gastroesophageal Reflux Disease (GERD)
These conditions often require specific dietary modifications, with the Low FODMAP diet being particularly beneficial for IBS management.
Role of FODMAPs in IBS Symptoms
FODMAPs can trigger IBS symptoms through various mechanisms. These carbohydrates are poorly absorbed in the small intestine and rapidly fermented by gut bacteria.
This fermentation process leads to:
- Gas production
- Increased water content in the bowel
- Distension of the intestinal walls
For individuals with IBS, these effects can cause significant discomfort. Bloating, abdominal pain, and altered bowel habits are common results of consuming high FODMAP foods.
By reducing FODMAP intake, many people with IBS experience relief from their symptoms. However, sensitivity to FODMAPs varies among individuals.
The Phases of Low FODMAP Diet
The Low FODMAP diet consists of three distinct phases:
Elimination Phase: All high FODMAP foods are removed from the diet for 2-6 weeks. This allows symptoms to settle and provides a baseline for comparison.
Reintroduction Phase: High FODMAP foods are systematically reintroduced one at a time. This helps identify specific trigger foods and individual tolerance levels.
Maintenance Phase: A personalized diet is created based on the results of the reintroduction phase. It includes as many FODMAP-containing foods as can be tolerated without triggering symptoms.
Each phase requires careful planning and monitoring. Working with a healthcare provider or registered dietitian is recommended for best results.
Setting Up Your Kitchen for Success

A well-organized kitchen is crucial for successfully following a low FODMAP diet. Proper setup enhances efficiency, reduces cross-contamination risks, and simplifies meal preparation.
Essential Kitchen Tools and Equipment
Invest in quality tools specifically for low FODMAP cooking. A set of color-coded cutting boards helps prevent cross-contamination between food groups. Sharp knives, measuring cups, and spoons ensure accurate portion control.
A food processor or blender is invaluable for creating FODMAP-friendly sauces and dips. Consider purchasing a garlic press for infusing garlic-flavored oil, a low FODMAP alternative to whole garlic.
Stock up on airtight containers in various sizes for storing prepared meals and leftovers. Glass containers are ideal as they don’t absorb odors or stains.
Organizing for Easy Access and Efficiency
Arrange your kitchen to streamline low FODMAP meal preparation. Group similar items together and store frequently used tools within easy reach.
Dedicate a specific pantry shelf or cabinet to low FODMAP ingredients. Label containers clearly with contents and expiration dates. Use clear storage bins to keep small items organized and visible.
Create a designated area for meal planning materials, including recipes, shopping lists, and FODMAP reference guides. This central location simplifies menu creation and grocery shopping.
Preventing Cross-Contamination
Implement strict measures to avoid mixing low and high FODMAP foods. Use separate utensils, cutting boards, and preparation areas for different food groups.
Clean all surfaces thoroughly between preparing different ingredients. Consider using disposable gloves when handling high FODMAP foods to prevent accidental transfer.
Store low FODMAP foods on upper shelves in the refrigerator and pantry to prevent drips or spills from contaminating them with high FODMAP items. Use sealed containers to further protect ingredients.
Clearly label all prepared foods with ingredients and date of preparation. This practice helps track meals and ensures everyone in the household can identify safe options.
Selecting Low FODMAP Ingredients

Choosing the right ingredients is crucial for successfully following a low FODMAP diet. Careful selection of foods can help manage symptoms while maintaining a balanced and nutritious eating plan.
Understanding FODMAP Content in Foods
FODMAPs are fermentable carbohydrates found in various foods. Some foods are naturally low in FODMAPs, while others contain high levels. Fruits like bananas, blueberries, and oranges are generally low FODMAP. Vegetables such as carrots, bell peppers, and spinach are safe choices. Meats, fish, and eggs are typically FODMAP-free.
It’s important to be aware of serving sizes, as some foods may be low FODMAP in small amounts but high in larger quantities. For example, avocados are low FODMAP at 1/8 of a whole fruit but become high FODMAP in larger servings.
Fruits, Vegetables, and Proteins
Low FODMAP fruits include strawberries, grapes, and kiwi. Safe vegetables include zucchini, tomatoes, and green beans. Proteins such as chicken, beef, and tofu are excellent low FODMAP options.
When selecting produce, opt for fresh or frozen varieties without added sauces or seasonings. For proteins, choose plain, unseasoned meats and fish. Avoid processed meats with additives that may contain high FODMAP ingredients.
| Low FODMAP Fruits | Low FODMAP Vegetables | Low FODMAP Proteins |
|---|---|---|
| Strawberries | Carrots | Chicken |
| Grapes | Spinach | Beef |
| Oranges | Bell peppers | Tofu |
| Kiwi | Zucchini | Eggs |
Grains and Dairy Alternatives
Many grains are low FODMAP and provide essential nutrients. Rice, quinoa, and oats are excellent choices. Gluten-free pasta made from rice or corn is a suitable alternative to wheat-based pasta.
For dairy alternatives, lactose-free milk and yogurt are available. Plant-based options like almond milk (unsweetened) and coconut yogurt are often well-tolerated. Hard cheeses such as cheddar and parmesan are naturally low in lactose and generally safe.
When selecting bread, look for gluten-free varieties or sourdough made from spelt flour, which is lower in FODMAPs than regular wheat bread.
Navigating Food Labels and Low FODMAP Products
Reading food labels is essential when following a low FODMAP diet. Look for ingredients that may indicate high FODMAP content, such as honey, high fructose corn syrup, or inulin.
Many products are now labeled as “low FODMAP certified.” These can be helpful, but it’s still important to check the ingredients list. Some common low FODMAP alternatives include:
- Garlic-infused oil instead of garlic
- Maple syrup instead of honey
- Tamari sauce instead of soy sauce
Be cautious with products labeled “gluten-free,” as they may still contain high FODMAP ingredients like apple fiber or inulin. Always check the full ingredients list to ensure the product fits within low FODMAP guidelines.
Mastering the Low FODMAP Meal Planning
Effective meal planning is crucial for success on a low FODMAP diet. It helps ensure nutritional balance, variety, and adherence to FODMAP restrictions.
Designing a Balanced Meal Plan
Create a weekly meal plan that includes a variety of low FODMAP foods. Focus on incorporating lean proteins, low FODMAP fruits and vegetables, and gluten-free grains. Aim for 3 main meals and 2-3 snacks per day.
Use a food diary to track meals and symptoms. This helps identify trigger foods and refine the meal plan.
Include a mix of carbohydrates, proteins, and fats in each meal. For example:
- Breakfast: Gluten-free oatmeal with strawberries and almond milk
- Lunch: Grilled chicken salad with mixed greens and olive oil dressing
- Dinner: Baked salmon with quinoa and roasted zucchini
Preparation Tips for Efficient Cooking
Batch cook low FODMAP staples to save time during the week. Prepare large portions of proteins, grains, and vegetables that can be easily combined for quick meals.
Stock the pantry with low FODMAP essentials:
- Gluten-free pasta and bread
- Canned tuna and salmon
- Low FODMAP snacks like rice cakes and nuts
Invest in meal prep containers for easy portion control and storage. Label prepared meals with dates to ensure freshness.
Low FODMAP Recipes and Cooking Ideas
Experiment with low FODMAP recipes to add variety to meals. Try:
- Stir-fries with tofu and low FODMAP vegetables
- Homemade soups using low FODMAP broths
- Frittatas with spinach and feta cheese
Adapt favorite recipes by substituting high FODMAP ingredients. Use garlic-infused oil instead of garlic, and lactose-free milk in place of regular milk.
Create a rotation of go-to meals for busy days. Keep ingredients on hand for quick options like:
- Rice bowl with grilled chicken and permitted vegetables
- Gluten-free wrap with turkey and lettuce
- Smoothie made with low FODMAP fruits and lactose-free yogurt
Shopping Strategies for Low FODMAP Diet
Navigating grocery stores on a low FODMAP diet requires planning and knowledge. Effective shopping strategies can simplify meal preparation and ensure adherence to dietary guidelines.
Creating a Low FODMAP Grocery List
A well-prepared grocery list is essential for successful low FODMAP shopping. Start by categorizing items into groups: proteins, vegetables, fruits, grains, and dairy alternatives. Include low FODMAP staples like:
- Proteins: Chicken, beef, fish, eggs, tofu
- Vegetables: Carrots, spinach, bell peppers, zucchini
- Fruits: Strawberries, blueberries, oranges, grapes
- Grains: Quinoa, rice, gluten-free oats
- Dairy alternatives: Lactose-free milk, almond milk
Keep this list handy on your phone or as a printed copy. Update it regularly based on meal plans and dietary needs.
Deciphering High and Low FODMAP Foods
Understanding which foods are high or low in FODMAPs is crucial. Use reliable resources like the Monash University FODMAP Diet app to check food statuses. Key points to remember:
- Portion sizes matter: Some foods are low FODMAP in small amounts but high in larger quantities
- Read labels carefully: Look for hidden FODMAPs in processed foods
- Be aware of FODMAP stacking: Consuming multiple low FODMAP foods can lead to a high FODMAP load
Create a cheat sheet of common high and low FODMAP foods to reference while shopping. This can help make quick decisions in the grocery store.
Budget-Friendly Shopping for a Low FODMAP Diet
A low FODMAP diet doesn’t have to break the bank. Here are strategies to keep costs down:
- Buy seasonal produce: It’s often cheaper and fresher
- Opt for frozen fruits and vegetables: They’re nutritious and have a longer shelf life
- Purchase in bulk: Stock up on non-perishable low FODMAP items when on sale
- Compare prices: Generic brands often offer low FODMAP options at lower costs
Plan meals around sales and discounts. Consider joining loyalty programs at your local grocery stores for additional savings. Preparing meals at home using whole ingredients is typically more cost-effective than buying pre-made low FODMAP products.
Personalizing Your FODMAP Diet

Tailoring the low FODMAP diet to individual needs is crucial for managing digestive issues effectively. This process involves careful tracking, systematic reintroduction of foods, and long-term adjustments to create a sustainable eating plan.
Tracking Food Intake and Symptoms
Keeping a detailed food diary is essential for identifying FODMAP sensitivities. Record all meals, snacks, and beverages consumed, along with any digestive symptoms experienced. Note the timing, severity, and duration of symptoms.
Use a smartphone app or notebook to log this information consistently. Include portion sizes and specific ingredients to enhance accuracy. Track stress levels and other factors that may impact digestive health.
This data helps pinpoint potential triggers and patterns in IBS symptoms. It also aids healthcare providers in assessing the effectiveness of the low FODMAP approach for each individual.
Reintroduction and Identifying Triggers
The reintroduction phase is critical for determining specific FODMAP sensitivities. Systematically reintroduce high FODMAP foods one at a time, starting with small amounts and increasing gradually.
Follow this process:
- Choose one FODMAP group to test
- Consume a small amount of the test food
- Monitor symptoms for 1-3 days
- If no symptoms occur, increase the portion and retest
- Move to the next FODMAP group after completing the test
Record reactions to each food carefully. This helps identify which FODMAPs trigger symptoms and in what quantities. Some people may tolerate certain high FODMAP foods better than others.
Adjusting the Diet for Long-Term Management
After identifying trigger foods, create a personalized long-term eating plan. Focus on including a variety of low FODMAP foods to ensure adequate nutrient intake and prevent deficiencies.
Consider working with a registered dietitian to develop a balanced diet that meets individual nutritional needs. They can help address concerns about nutrient deficiencies common in restrictive diets.
Regularly reassess tolerance levels, as sensitivities may change over time. Gradually reintroduce well-tolerated foods to expand dietary variety. This approach helps maintain gut health while managing symptoms effectively.
For those with inflammatory bowel disease or SIBO, additional dietary modifications may be necessary. Consult with healthcare providers to address specific concerns related to these conditions.
Living with a Low FODMAP Diet
Adopting a low FODMAP diet requires lifestyle adjustments and ongoing management. Strategies for dining out, accessing resources, and maintaining gut health are essential for long-term success.
Handling Dining Out and Social Situations
Dining out on a low FODMAP diet can be challenging but not impossible. Research restaurant menus in advance and look for simple dishes with grilled meats, fish, or eggs paired with low FODMAP vegetables. Ask servers about ingredient details and request modifications if needed.
When attending social gatherings, offer to bring a low FODMAP dish to share. Communicate dietary needs to hosts in advance. Eating a small meal before events can help manage hunger and reduce temptation.
For travel, pack low FODMAP snacks like nuts, rice cakes, and fruits like grapes or oranges. Research local grocery stores at your destination for suitable options.
Educational Resources and Support
The Monash FODMAP app is a valuable tool for identifying low and high FODMAP foods. It provides serving size recommendations and is regularly updated with new foods.
Low FODMAP cookbooks offer recipe inspiration and meal planning guidance. Look for titles by registered dietitians specializing in IBS and FODMAP diets.
Online forums and support groups connect individuals following the diet. These communities share tips, recipes, and emotional support.
Some hospitals and clinics offer low FODMAP diet classes or workshops. These sessions provide hands-on learning and personalized advice from dietitians.
Continuing Symptom Relief and Gut Health Maintenance
After the elimination and reintroduction phases, many find a personalized version of the low FODMAP diet provides ongoing symptom relief.
Regular exercise supports gut motility and overall health. Aim for 30 minutes of moderate activity most days of the week.
Stress management techniques like meditation or yoga can help reduce IBS flare-ups. Adequate sleep is also crucial for gut health.
Probiotic supplements may benefit some individuals. Consult a healthcare provider for recommendations on strains and dosages.
Stay hydrated by drinking plenty of water throughout the day. Limit caffeine and alcohol intake, as these can trigger symptoms in some people.